Crohn’s, Celiac or Ulcerative Colitis: 15 Years Symptom-free
Many years ago, my daughter started to suffer acute abdominal discomfort, bloating, gas and weight loss. After a few visits to the doctor and then a barium enema and subsequent X-ray, she was diagnosed with Crohn’s disease. Because Crohn’s is considered to be an inflammatory bowel disease with potentially serious side effects (such as having a bowel resection to remove badly inflamed, lesioned and/or necrotic tissue), the doctor we were seeing put her on an ASPIRIN® derivative called Pentasa (5-ASA) to combat the inflammation.
I was concerned enough to start doing research on Crohn’s and finding out all I could, including getting advice from a naturopath and homeopath. As an experimental psychologist, my philosophy has always been to research whatever seems reasonable and has some history of success. The naturopath suggested I buy a book, Breaking the Vicious Cycle, written by a Canadian woman, Elaine Gottschall.
Does the Gluten and Sugar-free Diet Work for Many types of IBD?
On first reading, the suggestions in Elaine Gottschal’s book seemed impossible to follow. I would have to go through every item in my cupboard and fridge, examine the labels, and if it had wheat, dairy, sugar or any form of gluten (this includes most of the grains except rice) then I was to throw it out and start fresh. That was the bad news. The good news was that Ms. Gottschall affirmed that most inflammatory bowel disease could be attributed to the start of inflammation from the by-products of ingestion of certain foods. A change in diet could potentially cure this by eliminating the by-products and thus the intestinal inflammatory response. The only caveat was that if the person had been on prednisone, the diet was not likely to work.
I can attest to the fact that very few prepared foods of any kind are free of wheat and/or dairy and/or sugar, never mind gluten. If you have never examined the ingredients on boxes, cans and even packages of product, you will be surprised. Even some labels of tomato sauce – tomato sauce for heaven’s sake – have sugar in them and ketchup is loaded with it.
My daughter was a typical young Canadian school girl at the time – she loved hamburgers, French fries, and – unbeknownst to me because I never had them in the house – any kind of sweets containing sugar. The sweets she would sneak or buy when she was at school.
I was a single working mom, usually tired when I came home from work. It seemed that I could never have the energy or time to make every meal from scratch. Standard items like bread and cold cuts to make sandwiches for lunch were off the menu, ice cream was off the menu, pizza off the menu, fried foods off the menu, mac and cheese off the menu, hot dogs (yes, hot dogs – if you examine the ingredients you will see that some brands have wheat and/or sugar) off the menu, ketchup definitely off the menu, pasta off the menu, yogurt off the menu (too much lactose in commercial yogurts, I would have to make my own), but fresh fruit and meats were allowed, thank God, and so were nuts. We were going to turn into rabbits and/or squirrels. The list seemed long and exhausting.
I usually had a mound of fruit and vegetables in my shopping cart. It was the “no wheat” clause that scared me the most. No bread. No rye, pumpernickel, linseed, challah, crusty baguette, sourdough or anything else. I love bread! Even pizza. We did not have pizza that often but now that it was off the menu I was in love with it. Impossible to let go of pizza.
As I kept debating on making this enormous change in diet, I was also calling our doctor because my daughter was not feeling better in spite of the Pentasa. She had constant gas, bloating, diarrhoea and pain. I read somewhere that perhaps high doses of Pentasa could create gas and asked the doctor about this. He wasn’t sure. And then we had a crisis.
Emergency Run to the Hospital at 5 A.M.
One night my daughter woke up screaming. We bundled her up, carried her to the car and raced to hospital emergency.
During the course of seven hours of waiting, tests and more waiting, all her vital signs started to plummet. My daughter was dying. All I could do was stand by her and hold her feet. They were ice cold. I have never held on to someone’s feet so fiercely and for such a long time. I was not going to let her go.
I did not let go of her feet until the stretcher was almost at the operating room door and then I went out and walked the streets because I could not bear to sit still.
They worked on her for four hours. I was back at the hospital watching the operating room door when the resident came out. He walked towards me. I stood up and did not want to cry.
He said, “She’s fine. She had acute inflammatory appendicitis which abscessed and then burst. It took us over two hours just to clean her bowels of the infection. But she’s fine.”
I was so overwhelmingly happy I burst into tears and then I threw my arms around him.
“And by the way,” he said casually before he left, “There was no sign of Crohn’s that I could see. There was massive infection but I saw nearly all of her intestines when we were washing them and there was no sign of Crohn lesions anywhere.”
So I went to see the radiologist with the X-rays which he had taken before he diagnosed my daughter with Crohn’s. I told him that she nearly died of acute inflammatory appendicitis and that there was no sign of Crohn’s. “How did you miss the appendicitis?” I asked. His only response was that her appendix had been hidden behind her intestine and that he was right, she had Crohn’s. “But she nearly died,” I said, “because you missed the appendicitis.” “You’ll see I’m right,” he said. I walked away.
Wake-Up Call
While my daughter recuperated in the intensive unit for a week, she was fed by IV. This is actually a good thing in the case of acute bowel inflammation because it allows the bowel to rest and heal without added irritants. And the antibiotics she was given were dealing with the infection.
Halfway through the week, a hospital nutritionist met with me and outlined the diet plan for someone with Crohn’s. Bland diet. White bread. White rice. I don’t remember the rest because I was horrified at what was considered to be an appropriate diet.
But I said nothing because I was determined that my daughter would start to follow Elaine Gottschall’s diet plan. The minute she was taken off the IV, I made two hospital runs a day with homemade chicken broth into which I had scrambled an egg. Bland but at least it wasn’t white marshmallow bread. Then I went home, bought a small chest freezer, threw everything suspect out of my cupboards and waited to bring my daughter home.
IBD Specialists Don’t Necessarily Believe in Diets
At the same time I made an appointment with an IBD specialist. I still felt we could use all the information and help we could get. The appointment, when it finally arrived, did not go well. He was a specialist who was doing some test runs on a new drug. “What will this drug do?” I asked. “She will have 30% fewer episodes of Crohn’s inflammation,” he said. “But what about diet?” I asked. “Isn’t diet important? I’ve read a report that says…” “It’s about quality of life,” he interrupted. “Okay,” I said. “What I understand you are saying is that she can eat anything she wants, including ice cream and fries and she will have 30% fewer episodes of sitting on the toilet with acute stomach pain?” “Yes,” he smiled.
As we walked out of his office, my daughter was still convinced that life was not worth living without fries. But I remembered that one of our babysitters ended up with a colostomy bag because of Crohn’s and so I stopped and said, “I can’t follow you around to make sure you stay on this diet. So you have a choice. You can either follow it and see what happens or you can have 30% fewer painful episodes of sitting doubled over on the toilet. I’m not being mean. It’s your choice, I promise. But I really, really hope you’ll think this over carefully before you choose.”
It took six months of experimenting and assembly line cooking on both our parts. When I cooked, I would make enough to freeze so we could manage for the month if we were lucky. I made eight loaves of almond bread at a time, six casseroles of eggplant and meat lasagne, stuffed zucchini, almond flour muffins (which disappeared in a day), vegetable meat loaf. It became easier and easier to get the hang of gluten- and sugar-free eating as we went along.
Soon we had people coming to my daughter for advice on how to manage such a diet. Whether she had Crohn’s or celiac disease, we never found out because she refuses to go through another barium enema to this day. But the diet works for many types of IBD according to Gottschall, so it may not matter what the exact diagnosis really was. And my daughter has not looked back. Today she is tall, straight and strong and, as long as she keeps away from gluten, wheat, milk, cream and soft cheeses, she is symptom-free.
If you are experiencing any of the symptoms discussed in the story above or any other gastric, stomach or colon pain or discomfort, contact the office of Dr. Vikram Tarugu to make an appointment as soon as possible.
The post Discovering My Daughter’s Colon Disorder and Getting Symptom Free appeared first on Gastroenterologists In Florida.
from
http://gastroinflorida.com/discovering-daughters-colon-disorder-getting-symptom-free/

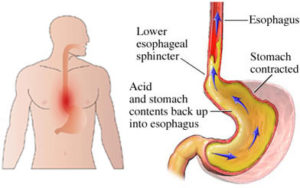 Symptoms of heartburn include a pain or burning sensation in the chest or throat area. Heartburn is initiated when acid from the stomach is released up into the esophagus which is the tube that runs from the mouth to the stomach. While heartburn for most people tend to be a “once in a while” experience, regular occurrences (two times or more per week) could potentially be a sign of a serious condition called “
Symptoms of heartburn include a pain or burning sensation in the chest or throat area. Heartburn is initiated when acid from the stomach is released up into the esophagus which is the tube that runs from the mouth to the stomach. While heartburn for most people tend to be a “once in a while” experience, regular occurrences (two times or more per week) could potentially be a sign of a serious condition called “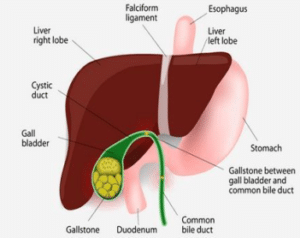 The gallbladder (a small organ inside of the stomach), is the place where gallstones (hard nuggets) develop and can vary in size from the size of grain of sand to the size of a golf ball (there can be multiple sizes at once).
The gallbladder (a small organ inside of the stomach), is the place where gallstones (hard nuggets) develop and can vary in size from the size of grain of sand to the size of a golf ball (there can be multiple sizes at once).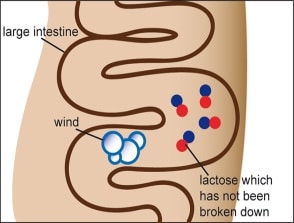 While being a common disorder, being “Lactose Intolerant” means that your body does not produce enough protein lactase to either break down or digest the content found in dairy products. Common symptoms of being lactose intolerant include bloating, stomach pain, gas and diarrhea after consuming dairy products (symptoms may not occur for 2-3 hours after consuming dairy products).
While being a common disorder, being “Lactose Intolerant” means that your body does not produce enough protein lactase to either break down or digest the content found in dairy products. Common symptoms of being lactose intolerant include bloating, stomach pain, gas and diarrhea after consuming dairy products (symptoms may not occur for 2-3 hours after consuming dairy products). Celiac Disease is involved with and targets the immune system and causes damage to the individual’s small intestine. This is typically a hereditary/genetic condition and requires individuals to not consume foods that contain “gluten”. Gluten is a certain type of protein that is found in barley, rye and wheat and if you experience pain or diarrhea after consuming foods with these proteins then you may have Celiac Disease.
Celiac Disease is involved with and targets the immune system and causes damage to the individual’s small intestine. This is typically a hereditary/genetic condition and requires individuals to not consume foods that contain “gluten”. Gluten is a certain type of protein that is found in barley, rye and wheat and if you experience pain or diarrhea after consuming foods with these proteins then you may have Celiac Disease.