Definition

What are Probiotics and their benefits to Gut?
Probiotics are the microorganisms that are beneficial for the deliberate manipulation of the intestinal micro flora. They are stated to be natural methods for disease control and healing, since they don’t generate the side effects like the antibiotics. At the same time they are stated to be more powerful than the other two methods of probiotics and the fecal transplant.
Probiotics Sources
The known sources of probiotics are the foods, cultured milk products, stains of lactic acid bacilli, Escherichia coli, Clostridium butyricum, Streptococcus salivarius, and Saccharomyces boulardii.
Probiotics Research
Scientists are conducting advanced researches on the genetically engineered bacteria that can have positive influence on the human immune system.
Reasons to take probiotics

Intestinal Micro Flora
The primary goal is to eliminate/deactivate the harmful bacteria that cause diseases. The other reasons to take probiotics are to enable the secretion of immuno-modulators for improving natural immunity, and to prevent the recurrence of diseases and disorders that have the root causes in the intestinal micro flora.
- Overcome Resistance: Certain species of the intestinal micro flora / pathogens can develop antibiotics resistance. Then the efficacy of the antibiotics will be diminished considerably. In such cases the scientists will have to change the ingredients, concentration, and try the other methods. The Probiotics have no such limitations.
- Avoid/reduce Side Effects: The consistent consumption of antibiotics can lead to many side effects. For example, the probiotics can reduce the infections to the respiratory tracts and diarrhea conditions. Probiotics also reduce the need for using the antibiotics to prevent the secondary levels of infections.
- Improved Barrier Performance: The intestinal epithelium acts as the natural barrier for filtering the various types of foreign-antigens, bacteria, and their toxic byproducts. The probiotics can improve the performance of the barrier. The first benefit is the tightening of the epithelial junctions. It is achieved by the synthesis of proteins to strengthen the junctions. The second benefit is the protection of the gut-barrier. They also defend the epithelium from pathogen attacks. The third benefit is the prevention of toxic elements accumulation in the intestine that may lead to diseases like the inflammatory bowels, Celiac, gastrointestinal disorders and the alcoholic liver.
- Pain Reduction/Modulation: Most of the intestinal disorders and diseases cause unbearable pain in the intestine, liver, kidneys, uterus (female), lower back, and the connected internal organs and the muscles. The Probiotics can generate the numbing effects by interacting with the CB1and CB2 receptors that are present in the brain, liver, kidney, intestine, and the other organs to reduce / suppress the sensations of pain. In many cases they perform the functions of the cannabinoid.
- Improved Immunity: Probiotics can induce the effects of natural immunity into the human body by interacting with the secretion of the Immuno-modulators. They can increase the strength and the efficiency of the immunity systems. The interleukin-10 and the trefoil factors (TFF) are some of them secreted by the probiotics. Breast milk contains large concentration of the TFF which can protect the newborn infant from many of the diseases and disorders. Hence, the medical experts strongly recommend breastfeeding for the babies.
Are Probiotics Good for You
Benefits of Probiotics
The medical reasons to take probiotics are many, including the healing of diseases caused by the intestinal micro flora. The biggest benefits are the secretion of the Probiotics proteins and DNA. They can alter the behavior of the harmful bacteria and the pathogens.
Benefits
The probiotics differ in their function from the antibiotics in the way they interact with the pathogens and the harmful bacteria. Instead of trying to kill or suppress, they alter the primary behavior of the pathogens which cause the diseases and disorders.
- Diarrhea Cure/Prevention: Diarrhea can cause dehydration in the children and the adults. It can also lead to other intestinal and internal organs infections and diseases. Probiotics can naturally heal the symptoms and prevent the effects of the pathogens from causing harmful side effects. They can cure the body from the effects of various types like the infectious diarrhea, rotavirus diarrhea, and the other diarrheal illness like the Collagenous colitis.
- Constipation Cure: One of the most regularly affecting disorders for the children, teens, adults, and the elders is the constipation. The Probiotics can restore the defecation frequency and the stool consistency to the normal conditions.
- IBS Cure: Probiotics are highly helpful for the curing of irritable bowel syndrome. The efficacy of the treatment is seen more in the experience of the healing effects by the patients.
Representation of Probiotics in the Gut (Human Digestive System)
The biggest benefit of using the Probiotics is the long term suppression of the incurable disorders like the alcoholic liver conditions. Experience has shown that the consumption of the antibiotics only suppresses the effects for a short span of time. The probiotics on the other hand can restructure the intestinal flora which is responsible for the further damages caused to the liver. They preserve the existing health conditions of the liver without letting them deteriorate further. Meanwhile, the patient can try and improve the conditions of the intestine and live through abstinence, diet management, and hydration of the intestine and the liver. Similarly, the probiotics provide healing for many other incurable infections, diseases and disorders.
Note
The treatments using the probiotics can benefit many of the patients suffering from allergy, H. pylori infection, mesenteric ischemia, hepatic encephalopathy, etc. The scientists are engaged in culturing new stains of the Probiotics for the advanced and chronic stages of the diseases.
Which is the Best probiotic?
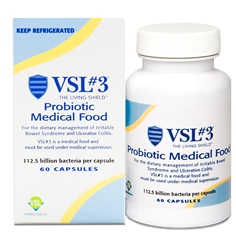
One of the best Probiotics – VLS#3
The determination of which is the best probiotic depends on the type of disease for which you seek treatment. There are many parameters involved in the selection of the best Probiotic. For example, they may include the specific disease, at a specific intensity, at a specific stage, and at specific health and immunity conditions for a specific patient. However, we can name a few of the probiotic which have been found to be efficient and effective. They are the VSL#3, Align (B. infantis), Culturelle (L. rhamnosus GG), DanActive (L. casei), Mutaflor (E. coli Nissle 1917), and Florastor (S. boulardii).
The post What are probiotics? Which is the best probiotic? How do you take them? appeared first on Gastroenterologists In Florida.
from
https://gastroinflorida.com/blog/what-are-probiotics-and-their-benefits/